HOME > Japan SPOTLIGHT > Article
Alzheimer's Disease: the Flagship Illness of a Greying World
By Anjana Ahuja
Introduction
It all started in 1901 with a hospital patient called Auguste Deter. The 51-year-old German woman was admitted to an asylum suffering from paranoia, aggression, disturbed sleep, confusion and memory loss. She deteriorated rapidly, and died five years later.
Her doctor, intrigued by her strange behavior, examined her brain after death. Dr. Alois Alzheimer published details of the "peculiar severe disease process of the cerebral cortex" that he had observed. It is thought to be the first known report of Alzheimer's disease, although the condition did not acquire the name of its discoverer until several years afterwards. The National Institute on Aging in the United States now describes Alzheimer's as an "irreversible, progressive brain disorder that slowly destroys memory and thinking skills, and eventually the ability to carry out the simplest tasks."
Today, Alzheimer's disease is a leading cause of dementia around the globe. Dementia is a cluster of symptoms associated with the loss of cognitive function and behavioral ability. It impairs a person's ability to think, remember and reason. There is currently no cure.
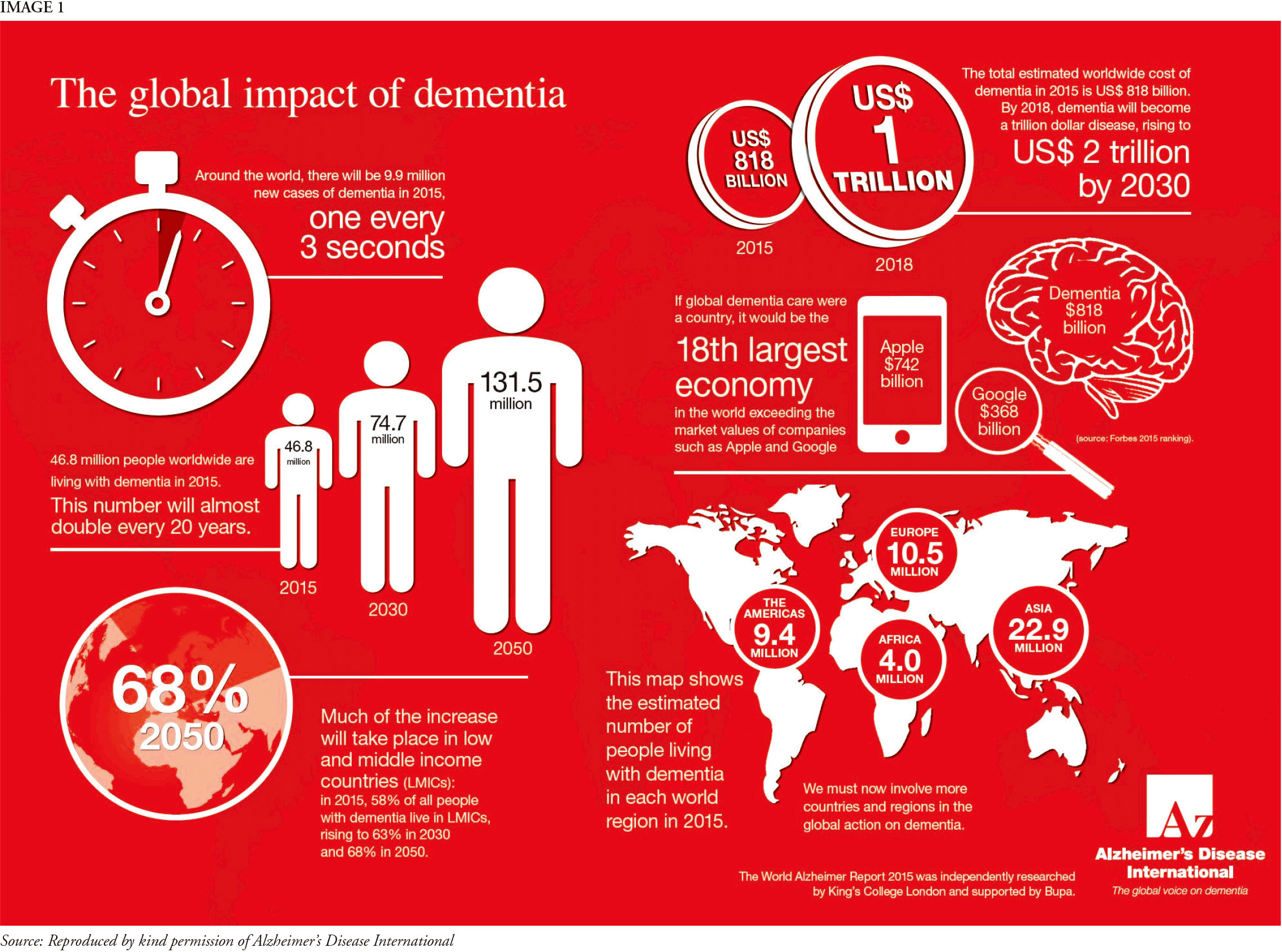
According to the World Alzheimer Report 2016, compiled by a team led by Prof. Martin Prince at the Global Observatory for Ageing and Dementia Care at King's College London, an estimated 47 million people around the world are living with dementia, and many have never received a formal diagnosis. Alzheimer's causes an estimated three out of five cases of dementia and has become the flagship illness of a greying world.
In 2015, the Population Division of the United Nations published a report entitled World Population Ageing, setting out some of the key trends and statistics in global demographics. The report says that population aging - a specific term that refers to the increasing share of older people in the population - is "poised to become one of the most significant social transformations of the twenty-first century, with implications for nearly all sectors of society, including labour and financial markets, the demand for goods and services, such as housing, transportation and social protection, as well as family structures and intergenerational ties."
Demographics of a Greying World
The 2015 UN World Population Ageing report defines "older people" as those aged over 60. Between 2015 and 2030, the number of older people will rise to 1.4 billion, and by 2050 it will be 2.1 billion. According to the World Health Organisation (WHO), the proportion of people aged over 60 is growing faster than any other age group, as a result of both longer life expectancy and declining fertility rates. The rapidly growing number of people living into old age is a healthcare success story but it generates new challenges. Diseases associated with aging, such as Alzheimer's, will become more widespread.
The ranks of the "oldest-old" will also expand: there were 125 million people aged over 80 in 2015. This is projected to grow to 434 million by 2050. This is partly due to medical advances but it also reflects the aging of baby boomers, a particularly large cohort of infants born after World War II. This means that by 2050, one in five older people will be over 80.
These demographic trends are the perfect vehicle for Alzheimer's. Let us look at the facts and figures compiled in the US by the Alzheimer's Association, which makes extensive reference to the work undertaken by Liesi Hebert, assistant professor at Rush University Medical Center in Chicago. One in nine people aged over 65 in the US has Alzheimer's. That rises to one in three for people aged over 85. Altogether, 81% of people who have Alzheimer's are aged over 75.
Developed countries such as Japan and the US, which boast high life expectancies, are already seeing big rises in the incidence of Alzheimer's. Collectively, dementia is thought to affect around 4.6 million people in Japan, with the figure expected to rise to 7 million by 2025. Lower and middle income countries will catch up in the coming decades, as their life expectancies increase.
What Causes Alzheimer's Disease?
There are two biological hallmarks of the disease, both caused by the build-up of malformed proteins in the brain. The first hallmark is abnormal clumps of sticky protein, called amyloid plaques. The second is tangled bundles of fibres, now called neurofibrillary tangles (or tau tangles). These plaques and tangles are thought to interfere with the smooth functioning of neurons, causing the cognitive problems associated with Alzheimer's. As the plaques and tangles build up, the condition worsens.
Both abnormalities are detected post-mortem, so a definitive diagnosis can only be made after death. The key to understanding Alzheimer's - and developing treatments - is thought to lie with these two proteins, amyloid and tau. Until recently, most efforts have focused on sticky amyloid plaques. This approach, however, has been relatively unsuccessful at generating new therapies.
Importantly, some people who never show symptoms of Alzheimer's during their life also turn out to have plaques on their brains. Some observers suggest that plaques might not cause the disease but merely be correlated with it. There may, in fact, be another primary disease-causing factor underlying both tau tangles and amyloid plaques.
It is unclear what triggers the build-up of plaques and tangles, but Alzheimer's and other forms of dementia are thought to arise through a complex interplay of genes and environment. Scientists suspect a genetic contribution to Alzheimer's because early-onset familial Alzheimer's disease (FAD) runs in families and is closely associated with single-gene mutations on chromosomes 21, 14 and 1. FAD strikes between the ages of 30 and 60, and accounts for about 5% of all Alzheimer's cases. The remaining 95% of cases are late-onset Alzheimer's, the age-related form with which we are most familiar and which we commonly refer to as Alzheimer's. Genetic testing cannot predict who will develop the disease in later life.
Existing Treatments
There is no cure for Alzheimer's. There are, however, several drugs licensed by the US Food and Drug Administration for treatment. These are not "disease-modifying" medicines - in other words, they do not alter the course or progression of the neurodegenerative disease. Rather, they treat the symptoms.
One class of medicines is called cholinesterase inhibitors. These medicines are designed to prevent the breakdown of acetylcholine, which is a messenger chemical in the brain that is crucial to memory and learning. This class of drugs helps the brain's nerve cells, or neurons, to keep communicating with each other.
Two - rivastigmine and galantamine - are prescribed for mild to moderate Alzheimer's. A third drug - donepezil, which is better known under its market name Aricept - can be prescribed at any stage. Their effectiveness varies between patients. A fourth drug, memantine, targets glutamate, which can damage brain cells.
The fifth drug is a combined therapy containing donepezil and memantine. Alzheimer's patients may also be offered non-medicinal therapies, such as cognitive behavior therapy or relaxation exercises.
Some drugs are still protected by patent, meaning that many people in low- to middle-income countries find them unaffordable. There may need to be a rethink on the pricing of anti-dementia drugs, as happened for lifesaving HIV drugs in Africa in 2000. Governments, supported by civil society, were able to radically push down prices and even enacted emergency laws to circumvent patent restrictions. There may be similar calls on dementia, especially if an effective therapy is discovered.
Treatments on the Horizon
Unfortunately, the history of Alzheimer's research is littered with drug failures. Towards the end of last year, Eli Lilly abandoned its large clinical trial of solanezumab, a compound designed to dissolve the amyloid plaques which are associated with Alzheimer's. The trial, the culmination of 15 years of research, was one of the biggest tests of the amyloid hypothesis - and it failed. In February this year, a large Merck trial of a drug named verubecestat proved similarly disappointing, with the company saying the trial was stopped because there was "virtually no chance of finding a positive clinical effect".
The journal Nature reported last year that several companies, including AbbVie, Bristol-Myers Squibb and Janssen, have anti-tau drugs in early-stage trials. We should, however, still be extremely cautious: the first late-stage clinical trial of a tau therapy, developed by Singapore-based TauRx Pharmaceuticals, has been less successful than hoped.
Some observers argue that researchers don't understand enough about the basics of dementia and Alzheimer's to come up with viable therapies. Dr. Amit Roy, from Foveal, a research company that advises on pharmaceutical investments, told the Financial Times in February this year: "All of these Alzheimer's drugs fail for the same reason. We do not understand the science of what causes Alzheimer's, and instead look at things associated with the disease in the hope that modifying them with drugs will modify the illness. Until drugmakers can do more than describing what changes happen in Alzheimer's and prove that a certain mechanism actually causes the disease, these drugs will keep failing - the science is too immature."
Economic Costs
The World Alzheimer Report 2016 estimates the total annual cost of dementia to currently be around $818 billion, and that it will become a $1-trillion disease by 2018. By 2030, it will become a $2-trillion disease. If dementia were a country, it would currently be the 18th largest economy in the world.
These are astonishing statistics. That is because dementia represents a double economic blow: it removes people from the labor market and it adds cost burdens in the form of healthcare interventions and social care. Dementia sufferers are often looked after by unpaid caregivers, such as their children or other family members, who are often themselves of working age and therefore represent further lost labor. Thus, the effects ripple outwards - socially, economically and generationally - far beyond those suffering from the disease.
In February 2016, a team of researchers led by Dr. Marcus Keogh-Brown, from the London School of Hygiene and Tropical Medicine, tried to calculate the likely economic effect of Alzheimer's on China, the second-largest economy in the world. The simulation, published in the journal EbioMedicine, predicted that, based on current rates of the disease and the aging of the population, there will be 28 million Chinese sufferers by 2050.
Inputting these numbers into a simulation of the Chinese economy yields a shocking economic blow by 2050: the macroeconomic costs due to Alzheimer's alone are predicted to reach $1.07 trillion by 2050. This is equivalent to China's total GDP in 2012. Around 62% of the economic impact is due to a depleted workforce (which loses both patients and caregivers) resulting in lost productivity. In short, dementia has the power to bankrupt economies.
A similar apocalyptic future is forecast for Japan. In 2014, Dr. Takaomi Saido, a leading scientist at Riken's Brain Science Institute, told the Japan Times that "Alzheimer's disease will destroy Japan's social welfare mechanisms in the near future." He believes that scientists should focus on prevention and effective treatments if a crisis is to be averted.
The Social Costs & Challenges of Alzheimer's
Alzheimer's is not just a medical emergency but a social one. All branches of society will have to adapt and change in response to a growing number of citizens with dementia.
In 2016, for example, a record number of people with dementia were reported missing in Japan, making it a very real issue for the police. According to the Guardian newspaper, around 12,200 Japanese patients had vanished, with some subsequently found dead. This, the newspaper reported, was a symbol of the looming social crisis caused by an aging population, with many families reporting that they could not monitor their sick relative around the clock and that such demands were becoming burdensome.
With its super-aging population, Japan has little choice but to become a pioneer in how it treats dementia sufferers. There is, for example, the Dementia Friendly Japan Initiative, a collaboration between universities, companies, charities and non-profit organizations, which promotes dementia-friendly public transport, and offers fragrance days to help people access some memories through smell.
Japan has also been working hard to create new inclusive communities, with dementia services built in from the beginning. These communities, such as Sanada in Ueda City, have group care homes and multifunctional care centers. They encourage social contact. There are also millions of "dementia volunteers" across the country, who can look out for elderly wanderers and provide social support in the community.
Other social issues include financial and legal planning for the future. Society needs to encourage older people and their families to have honest conversations about what should happen if dementia strikes. Preparing properly for dementia requires a great deal of administration: the drafting of wills, expressing wishes about medical treatment, granting power of attorney and dealing with property and other assets, especially if care is expensive.
There also needs to be discussion, within families and governments, about end-of-life care. Patients can live for a decade or more after diagnosis. In the final stages of dementia, they are unable to care for themselves and sometimes unaware of their environments. They lose autonomy, privacy and independence.
The rise in dementia prevalence is likely to spur discussions about assisted suicide and euthanasia. Many countries, including the United Kingdom, feel uncomfortable at the idea of legislating on the right to die, for reasons such as the sanctity of life and the belief that doctors have a duty to care, not kill. At present, the Netherlands is one of the few countries to allow people in certain circumstances, including a dementia diagnosis, to die with the help of a doctor. Canada, Luxembourg, Belgium and Switzerland have all enacted similar legal rights. In the UK, public opinion favors a right-to-die law but MPs do not.
In 2013, Taro Aso, the deputy prime minister of Japan, made headlines around the world when he suggested that the elderly "hurry up and die" to alleviate the burden of costly care. This started an important debate in Japan about whether its senior citizens should have more control over the end of their lives.
Response of Global Policymakers
Over the past few years, policymakers seem to have woken up to the demographic reality of an aging, dementia-riddled world. In 2013, the UK hosted the first G8 summit dedicated to dementia. In their declaration afterwards, G8 ministers pledged the following: to find a cure or disease-modifying therapy by 2025; to increase spending on research and enrol more patients in clinical trials; to develop an international action plan on research; and to encourage publication of all dementia research so that new avenues can be quickly identified.
Many countries have latched on to this timetable, specifying targets for 2025. Japan, for example, aims to have trained 60,000 primary care doctors in dementia diagnosis by 2025. The WHO drafted a global action plan on the public health response to dementia that was submitted to its Executive Board earlier this year.
How realistic is it that we will find a disease-modifying Alzheimer's drug by 2025? Dr. Jeffrey Cummings, a renowned Alzheimer's researcher affiliated with the Cleveland Clinic in Ohio, recently led an analysis of drug development in this field. In a paper published in September last year, in the journal Alzheimer's Research and Therapy, he estimated that - given the current research and licensing environment - it would take about nine years and $5.7 billion to develop such a therapy.
If the 2025 deadline were to be met, it would mean that any drug would have to be in early clinical trials now. Dr. Cummings counted around 70 compounds being researched right now but pointed out that many still target amyloid, a focus that has so far proved a flop. One way to expedite the process, he suggests, might be to shorten the time needed for clinical trials and licensing. Better diagnosis and more sensitive tests to detect cognitive decline may also help, especially when it comes to therapies that could potentially target mild Alzheimer's.
Medicines are not the only area of policy focus. The care of patients is critical. The World Alzheimer Report 2016 argues that dementia care is currently over-specialized, and that some of that care should shift to primary care providers, such as local doctors. Good-quality primary care can be scaled up relatively quickly and cheaply in tandem with the aging population, unlike the very specialized attention provided by geriatric doctors, neurologists and psychiatrists. Primary care can also provide an appropriate environment to tend to more general needs of dementia patients, such as help with nutrition and avoiding falls.
In the absence of an effective treatment, society also needs to consider assistive technologies. These can help patients to stay independent for longer. Such technologies already include automated pill dispensers, and sensors that can detect when someone has fallen or wandered beyond the boundaries of their home.
What About Prevention?
Prevention is said to be better than cure - and there is no cure for Alzheimer's and other forms of dementia. That makes prevention a hugely important topic for scientists and policymakers. It is important to remember that not every old person will succumb to dementia, and studies are currently underway to find out what differentiates sick older people from their healthy peers. There is some dispute as to the strength of the connection between lifestyle choices, such as exercise and diet, and dementia risk. Observational studies appear to show that a healthy lifestyle is correlated with a lower risk of cognitive decline and dementia.
For example, a paper published in June 2015 in the journal Alzheimer's and Dementia, lead-authored by Matthew Baumgarten, senior director of public policy at the Alzheimer's Association in the US, states: " ...[the Alzheimer's Association] believes there is sufficiently strong evidence, from a population-based perspective, to conclude that regular physical activity and management of cardiovascular risk factors (diabetes, obesity, smoking, and hypertension) reduce the risk of cognitive decline and may reduce the risk of dementia. The Association also believes there is sufficiently strong evidence to conclude that a healthy diet and lifelong learning/cognitive training may also reduce the risk of cognitive decline."
The National Institute on Aging in the US is more restrained: "So far, studies have not demonstrated that, over the long term, health or lifestyle factors can prevent or slow Alzheimer's disease or age-related cognitive decline." The institute is running around 30 clinical trials investigating this issue. Some researchers claim that brain training games can delay dementia but this is highly contested.
The Outlook for Alzheimer's
There may be some encouraging news on the horizon. Various recent studies suggest that dementia rates are falling in certain populations. In November 2016, a survey of around 21,000 people aged over 65 was published in the journal JAMA Internal Medicine. This paper showed that the proportion of people with dementia was 8.8%, compared to a rate of 11.6% in 2000.
Prof. Kenneth Langa from the University of Michigan, who conducted the study, told the BBC that "the decline in dementia risk is a real phenomenon" and said that education might be the key. Those reaching old age today tend to be better educated than earlier cohorts. The decline has been measured in other countries too, including the UK and Spain. Aspects that contribute to better overall health over a lifetime - such as childhood vaccinations, improved nutrition and reduced smoking - may finally be playing out in the realm of dementia.
We must not be complacent. But, after decades of gloom and with effective medicines still at least a decade away, this recent decline in dementia rates is a glimmer of hope in our greying world.
Japan SPOTLIGHT May/June 2017
(2017/05/18)
Anjana Ahuja
Anjana Ahuja is a freelance science writer in the UK and a contributing writer on science for the Financial Times. Twitter: @anjahuja

























