HOME > Japan SPOTLIGHT > Article
A Preventable Disaster: The Findings & Recommendations of the Independent Panel for Pandemic Preparedness & Response on Covid-19
By Jillian Yorke
The Age of Pandemics
"At the dawn of the 21st century, the world finds itself in an age of pandemics. Covid-19 is not the first pandemic – it will not be the last. It may not be long before the world faces the next one. The task at hand is to learn lessons at this stage of Covid-19 to strengthen the world's response to its next stage – and ensure we are all better prepared for future pandemics."

(Dr. Raj Panjabi, in a background paper for the IPPPR, presented in September 2020.)
Introduction
The Independent Panel for Pandemic Preparedness and Response (IPPPR), co-chaired by Helen Clark, former prime minister of New Zealand, and Ellen Johnson Sirleaf, former president of Liberia, was established by World Health Organization (WHO) Director-General Tedros Adhanom Ghebreyesus on July 10, 2020, in response to World Health Assembly Resolution 73.1. The Panel's mission was to analyze how a disease outbreak became a global pandemic; evaluate the national and global responses to the current pandemic, including those of the WHO; review lessons learned; and make recommendations on how to both better respond to the current pandemic, and prepare more effectively for future global health threats. The evaluation was fact- and evidence-based and the Panel, true to its name, is impartial and fully independent.
The Panel has 11 other members, who were appointed by the co-chairs and have considerable expertise and experience in areas such as infectious diseases, public health policy, outbreaks and emergencies, economics and financing, and gender issues. They represent neither their governments nor their institutions. The IPPPR also drew on the research, knowledge and skills of many other experts and concerned parties throughout the world. In its quest for truth, justice and reform, the Panel's mandate was vast and broad-ranging. Its final Report and recommendations are clear and bold, and will surely be transformative if fully implemented.
At its second meeting, in October 2020, the Panel laid out its four interconnected areas of focus:
"i. Build on the past: Learn from previous epidemics and pandemics and the status of the system and actors pre-Covid-19.
ii. Review the present: Determine an accurate and verified chronology of events and activities in relation to the Covid-19 pandemic; analyze recommendations made by the WHO and responses by national governments.
iii. Understand the impact: Review how health systems and communities responded, and assess the direct and indirect impacts of both the pandemic and response measures.
iv. Change for the future: Develop a vision for a strengthened international system ideally equipped for pandemic preparedness and response including both the WHO and the international system at large."
Over eight months, the IPPPR has conducted rigorous studies, utilizing multiple methods such as a review of existing literature, town hall-style meetings open to all, roundtable discussions, original research, the welcoming of submissions and contributions, and hearing directly from frontline workers. As a result, it "now has the most authoritative analysis of events yet produced". I have been following the Panel's work closely, and am impressed by its comprehensive scope, willingness to listen to and learn from numerous viewpoints, transparency, unstinting efforts, and evidence-based yet compassionate stance.
On May 12, 2021, the co-chairs presented the Panel's Main Report, Covid 19: Make it the Last Pandemic. A summary of the report, several background papers, and a detailed chronology of events were also released. At the end of May, the Panel presented its findings to the World Health Assembly. Below I highlight some of the findings and recommendations (Image).

Lessons from the Past not Learned
The Panel calls the Covid-19 pandemic "a disaster which could have been averted". Over the last 12 years, since the 2009 H1N1 influenza pandemic, there have been numerous high-level reports warning of an inevitable pandemic threat and urging improvements in global preparedness. Suggestions have included strengthening the role of the WHO and securing its better funding, and reforming the implementation of the International Health Regulations (IHR) – exactly what the current Panel recommends. However, these previous warnings and recommendations were mostly not implemented, and there was inadequate funding and preparedness testing, despite the increasing rate of zoonotic diseases. Ellen Johnson Sirleaf stressed that this time must be different: "The shelves of storage rooms in the UN and national capitals are full of reports and reviews of previous health crises. Had their warnings been heeded, we would have avoided the catastrophe we are in today."
February 2020: The Lost Month
In its comprehensive, detailed chronology of events since the pandemic started, the IPPPR describes February 2020 as "the lost month". Although the WHO knew of the emergence of a new virus in Wuhan, China in December 2019, it was not until Jan. 30, 2020 that it declared a public health emergency of international concern (PHEIC). At the time, outside China, there were fewer than 100 cases and no deaths. The Panel found that the WHO could have declared a PHEIC eight days sooner, in its earlier meeting. Moreover, it was only on March 11, 2020 (when there were a reported 118,000 cases in 114 countries) that the WHO, stating that it was alarmed by the extent of both the spread of the disease and the level of inaction in response, characterized Covid-19 as a global pandemic. Most countries did not take the threat seriously before then. The Report clarifies, "The failure of most countries to respond during February was a combination of two things. One was that they did not sufficiently appreciate the threat and know how to respond. The second was that, in the absence of certainty about how serious the consequences of this new pathogen would be, 'wait and see' seemed a less costly and less consequential choice than concerted public health action." This delay has had devastating consequences. As of late May 2021, there have been 164 million cases of Covid-19, and 3.4 million deaths.
Even after the declaration of the PHEIC, in a "cycle of complacency", there was no coordinated global response. It was only after Covid-19 had spread internationally and the number of cases increased substantially that governments took thorough-going action to prevent transmission. Further, while WHO advised of the possibility of human-to-human transmission in the period until it was confirmed, and recommended measures that health workers should take to prevent infection, the Panel's view is that it could also have told countries that they should take the precaution of assuming that human-to-human transmission was occurring.
What Worked, What Didn't
The Panel says, "The shared learnings about the successes in responding to Covid-19, and the hard-won lessons from failings, represent a once-in-a-lifetime opportunity to get preparedness right to prevent a catastrophic pandemic from arising again." It conducted in-depth analysis of the responses of 28 countries, and identified three strategic approaches: aggressive containment, suppression, and mitigation. Countries with aggressive containment include China, New Zealand, South Korea, Singapore, Thailand and Vietnam. Effective national responses featured clear decision-making authority, coordinated cross-sector efforts, adaptability, and the ability to provide timely science-based advice that was then followed. Leadership and competence have proved more important than a country's wealth.
Meanwhile, "countries with the poorest results in addressing Covid-19 had uncoordinated approaches that devalued science, denied the potential impact of the pandemic, delayed comprehensive action, and allowed distrust to undermine efforts. Many had health systems beset by long-standing problems of fragmentation, undervaluing of health workers and underfunding. They lacked the capacity to mobilize quickly and coordinate between national and subnational responses. The denial of scientific evidence was compounded by a failure of leadership to take responsibility or develop coherent strategies aimed at preventing community transmission. Leaders who appeared skeptical or dismissive of emerging scientific evidence eroded public trust, cooperation and compliance with public health interventions."
The IPPPR's analysis of over 80 countries found that orders to stay at home reduce the number of cases only when households have sufficient income to survive, people are able to work remotely (i.e., have digital access), and there is enough trust in the government for its orders to be obeyed. In regard to the WHO, the Panel says, "WHO staff worked extremely hard to provide advice and guidance, and support to countries, but Member States had underpowered the agency to do the job demanded of it."
Reform of the WHO
The Panel found that "the way the WHO is financed today has serious impacts on the quality of the organization's performance. Global health is inevitably a politically charged domain and it is vital that the WHO is strong enough to be able to perform with maximum independence." Among other things, the Panel recommends establishing the WHO's financial independence, strengthening the authority and independence of the director-general, empowering the WHO to take a leading role in an emergency response to a pandemic, equipping WHO Country Offices sufficiently to respond to technical requests from national governments to support pandemic preparedness and response, including support to build resilient equitable and accessible health systems, universal health care (UHC) and healthier populations, prioritizing the quality and performance of staff at each WHO level, and de-politicizing recruitment.
Regarding the pandemic alert system, the Panel states, "The bias of the current system of pandemic alert is towards inaction – steps may only be taken if the weight of evidence requires them. This bias should be reversed – precautionary action should be taken on a presumptive basis, unless evidence shows it is not necessary. In changing the system of alert to orient it towards speedy action, the incentive structures need to be addressed. At present, from local up to international level, public health actors only see downsides from drawing attention to an outbreak that has the potential to spread. Incentives must be created to reward early response action and recognize that precautionary and containment efforts are an invaluable protection which benefits all humanity."
Inequalities Revealed
Covid-19 has starkly revealed and exacerbated the existing problems and deeply embedded inequalities in our societies and health systems. It has had a disproportionate effect on women and vulnerable or marginalized groups. Up to 125 million more people are estimated to have been pushed into extreme poverty. Millions of children, especially the most disadvantaged, have had their education terminated. Social problems such as domestic violence, sexual abuse, and child marriage have all worsened considerably. In addition, the world lost US$7 trillion in GDP in 2020, the deepest shock to the global economy since World War II.
It has been a challenging time for those with non-communicable diseases (NCDs), such as diabetes or cancer. According to the NCD Alliance, more than one in five people have an underlying condition that gives them a greater risk of experiencing severe symptoms if they contract Covid-19. Charity Muturi of the NCD Alliance of Kenya says, "People have not realized that NCDs are just a slow pandemic." Moreover, access to medicines and hospitals for vital ongoing treatment has often been drastically curtailed by the pandemic. Many nations' health systems were already struggling to manage NCDs competently, even before the current pandemic. In a Zoom town hall-style meeting on NCDs organized by the Panel that I participated in on March 25, local communities and organizations all over the world shared their concerns as well as some of the many new public health initiatives that have been set up in response. These included addressing obesity, improving palliative care, building resilience, ensuring safe water supplies, expanding connectivity, bringing medications to patients' homes, and offering medical advice by telephone.
Another deeply disturbing issue brought up during this Zoom discussion was the relationship between "unhealthy commodity industries" (such as the tobacco, gun, and alcohol industries) and Covid-19. A report dubbed "Signalling Virtue, Promoting Harm" that analyzes the tactics and strategies that have been employed by such industries during the pandemic can be seen on the NCD Alliance website (https://ncdalliance.org).
Changing the Way We Eat
Another urgent area for reform is the way we produce food. In particular, according to many experts, industrial farming is a disaster waiting to happen, and a major risk factor for the occurrence of new pandemics, both viral (such as the coronavirus) and bacterial types (such as the bubonic plague). The way we cram food animals into tight spaces and their generally bad conditions increase their stress, while the overuse of antibiotics given to such animals leads to antimicrobial resistance, meaning that previously effective drugs may no longer work. Moreover, because they have been genetically bred for specific traits, these animals tend to be identical, enabling viruses to spread more easily. Indeed, there have been many examples in the past of zoonotic transmission to humans originating in animals bred for food, such as the H1N1 swine flu in 2009, which began in pig farms, and resulted in the deaths of hundreds of thousands of people. Sonia Shah, author of Pandemic (2017), calls crowded factory farms "ticking time bombs" because they could easily give rise to both virulent avian influenza and highly drug-resistant bacterial pathogens. Currently, about 90% of the global meat supply comes from such factory farms, which are also problematic in terms of climate change, cruelty to the animals they process, and harm to human health. For more on this topic, see The Omnivore's Dilemma by Michael Pollan (Bloomsbury, 2006), a book I found both highly informative and deeply disturbing.
The Chernobyl Moment
The Panel calls this "the Chernobyl moment for public health". In the same way that the Chernobyl nuclear disaster eventually led to more information exchange and openness on nuclear issues, and increased power being given to nuclear regulatory agencies, the current pandemic is a fundamental crisis that must produce greater global collaboration and data-sharing, as well as a strengthening of the WHO. "Our message for change is clear: no more pandemics. If we fail to take this goal seriously, we will condemn the world to successive catastrophes. At the same time, our careful scrutiny of the evidence has revealed failures and gaps in international and national responses that must be corrected. Current institutions, public and private, failed to protect people from a devastating pandemic. Without change, they will not prevent a future one. That is why the Panel is recommending a fundamental transformation designed to ensure commitment at the highest level to a new system that is coordinated, connected, fast-moving, accountable, just, and equitable – in other words, a complete pandemic preparedness and response system on which citizens can rely to keep them safe and healthy."
The Panel's recommendations fall into two categories: immediate measures to halt the current pandemic, and urgent global action and sweeping systemic change to prevent future pandemics. As well as every country applying proven public health measures "at the scale required to curb the pandemic", with strong leadership from heads of state and government, the Panel recommends that:
• High-income countries with a vaccine pipeline for adequate coverage should, alongside their scale-up, commit to provide to the 92 low- and middle-income countries in the COVAX Gavi Advance Market Commitment with at least one billion vaccine doses by September 2021 (Chart 1).
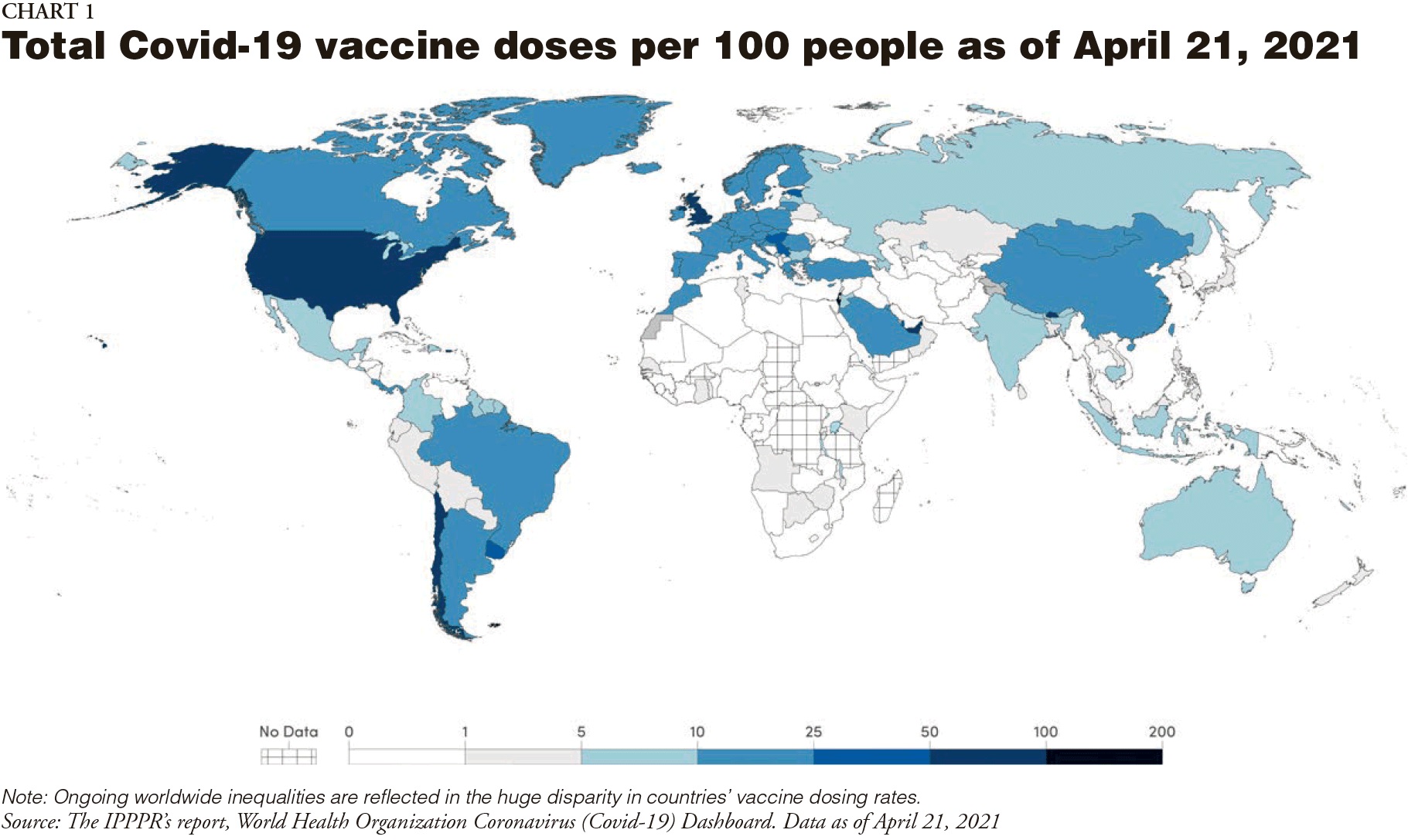
• Major vaccine-producing countries and manufacturers should convene, under the joint auspices of the WHO and the World Trade Organization (WTO), to agree to voluntary licensing and technology transfer. If actions on this don't occur within three months, a waiver of intellectual property rights under the Agreement on Trade-Related Aspects of Intellectual Property Rights should come into force immediately.
• The G7 should immediately commit to provide 60% of the $19 billion required for the Access to Covid-19 Tools Accelerator (ACT-A) in 2021 for vaccines, diagnostics, therapeutics, and strengthening of health systems, and a burden-sharing formula should be adopted to fund such global public goods on an ongoing basis.
An Equity-Centered Global Public Health Perspective
To prevent future pandemics, the Panel calls for a fundamental transformation of the global pandemic preparedness and response system through a package of bold reforms, including the following:
• Establishing a Global Health Threats Council that will maintain political commitment to pandemic preparedness and response and hold actors accountable, including through peer recognition and scrutiny. Countries should also adopt a Pandemic Framework Convention within the next six months.
• Establish a new global system for surveillance based on full transparency. This system would provide the WHO with the authority to publish information about outbreaks with pandemic potential on an immediate basis without needing to seek approval and to dispatch experts to investigate at the shortest possible notice.
• Invest in national preparedness now as it will be too late when the next crisis hits. All governments should review their preparedness plans and allocate the necessary funds and people required to be prepared for another health crisis.
• Transform the current ACT-A into a truly global platform aimed at delivering global public goods including vaccines, diagnostics, therapeutics, and supplies that can be distributed swiftly and equitably worldwide – shifting from a market model to one aimed at delivering global public goods.
• Focus and strengthen the authority and financing of the WHO, including by developing a new funding model to end earmarked funds and to increase Member State fees.
• Create an International Pandemic Financing Facility, which would have the capacity to mobilize long-term (10-15 year) contributions of approximately $5 to $10 billion per year to finance ongoing readiness. It would also be ready to disburse from $50 to $100 billion at short notice by front-loading future commitments in the event of a pandemic declaration. The Global Health Threats Council would allocate and monitor the funding to institutions which have the capacity to support the development of preparedness and response capacities.
• Heads of state and government should at a global summit adopt a political declaration under the auspices of the UN General Assembly to commit to these transformative reforms.
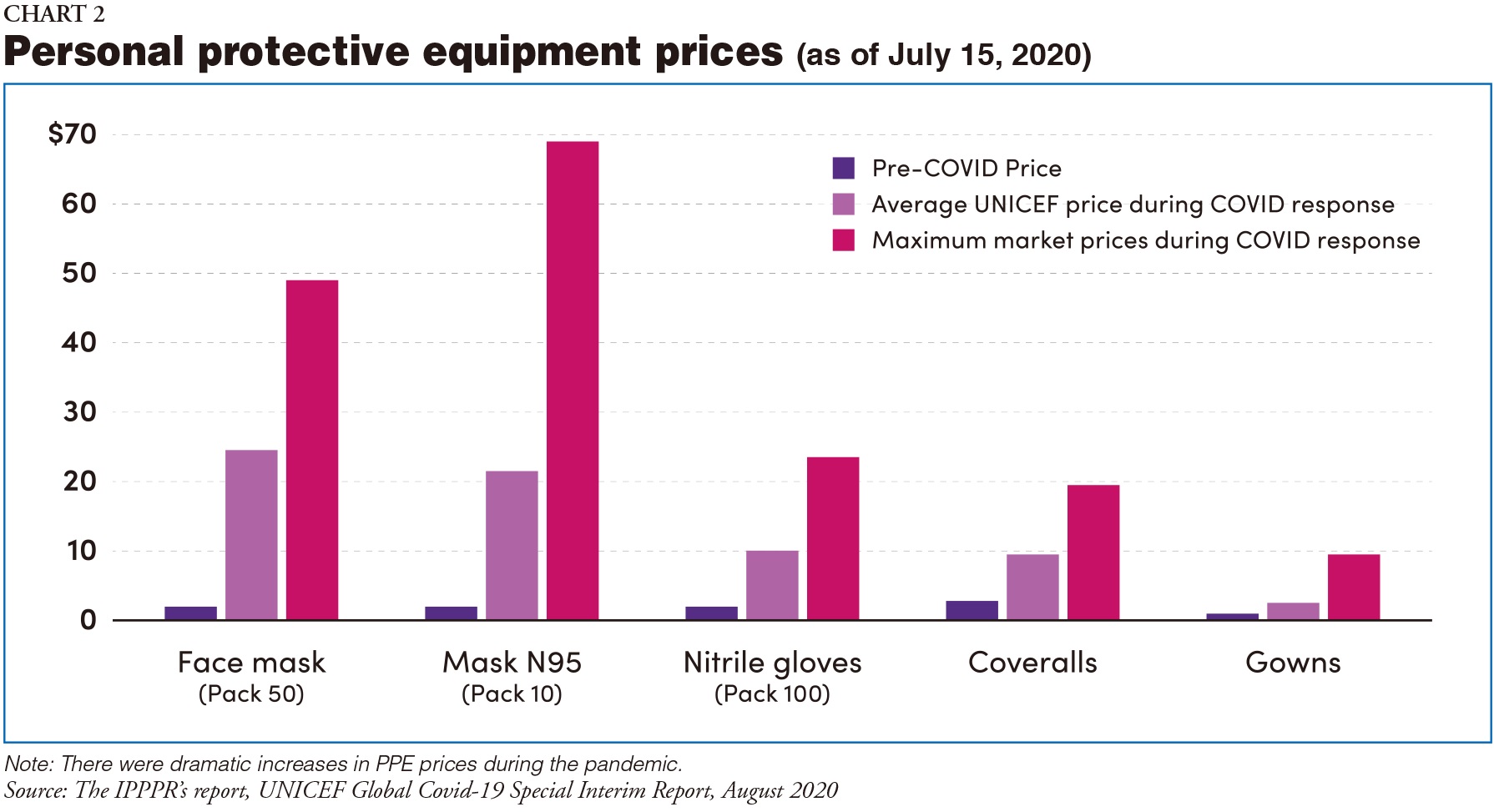
The Panel believes that it is in countries' own best interests to implement these recommendations. Helen Clark said, "The tools are available to put an end to the severe illnesses, deaths, and socio-economic damage caused by Covid-19. Leaders have no choice but to act and stop this happening again." Other experts mentioned the importance of getting private industry involved in reforms, the need for more equitable data-sharing, greater emphasis on global common goods, and the requirement to change from charity-driven models to models based on social justice (Chart 2).
Conclusion
Finally, the Report concludes: "The transformation of the international system for pandemic preparedness and response which the Panel recommends will fail if it is approached piecemeal. The lesson from previous recommendations for change following earlier pandemics is that change will only result from the adoption and implementation of inter-linked and interdependent measures. Just as pandemic preparedness itself is undone by failure in the weakest link in the chain, so too recommendations for change will fail if the hardest problems are set aside. The Panel has assessed the set of recommendations it has proposed against one criterion only: if they had been in place, would they have stopped the Covid-19 pandemic? We believe the answer is yes, and therefore urge their implementation as a whole and in a timely manner. The Panel's recommendations aim to equip countries and the international system to prevent an outbreak from becoming a pandemic and, if a pandemic does occur, to prevent it becoming a global health and socioeconomic crisis."
Note: To read the IPPPR Main Report, see: COVID-19: Make it the Last Pandemic (https://theindependentpanel.org/wp-content/uploads/2021/05/COVID-19-Make-it-the-Last-Pandemic_final.pdf)
The Image and Charts are taken from the IPPPR Main Report. The author would like to thank the Panel for its kind assistance.
Japan SPOTLIGHT July/August 2021 Issue (Published on July 10, 2021)
(2021/08/11)
Jillian Yorke
Jillian Yorke is a translator, writer and editor who lived in Japan for many years and is now based in New Zealand, where she is the Curator of the Japan Library: Pukapuka

Japan SPOTLIGHT

- Coffee Cultures of Japan & India
- 2025/01/27
























